How is your digestion these days? I’d be willing to bet if you are reading this, it’s not so great. The main remedy for indigestion is an acid-reducing pill, tablet or powder. Whether it’s over the counter or in prescription form, it’s still a band-aid.
How is your digestion these days?
I’d be willing to bet if you are reading this, it’s not so great.
The main remedy for indigestion is an acid-reducing pill, tablet or powder. Whether it’s over the counter or in prescription form, it’s still a band-aid.
Without investigating why you keep getting indigestion, heartburn or GERD, you’ll keep throwing your dollars away.
I like to save money whenever possible. How about you?
I prefer to spend my hard-earned dollars on things I enjoy rather that on things that patch me up for a limited time.
The way I see it, spending money on things like TUMS or even prescriptions to block the acid in my stomach are not only counter-productive, but a waste of money.
There’s also the actual danger of using these products for a prolonged period of time. You may feel better initially, but the long-term ramifications are much worse.
NOTE: Some diagnoses require the use of acid-blockers. Please consult your physician prior to stopping any medications you have been prescribed.
Below are 4 of the most common myths I see about stomach acid and digestion.
Let’s dive into each of these myths, shall we. (HCL= Stomach Acid)
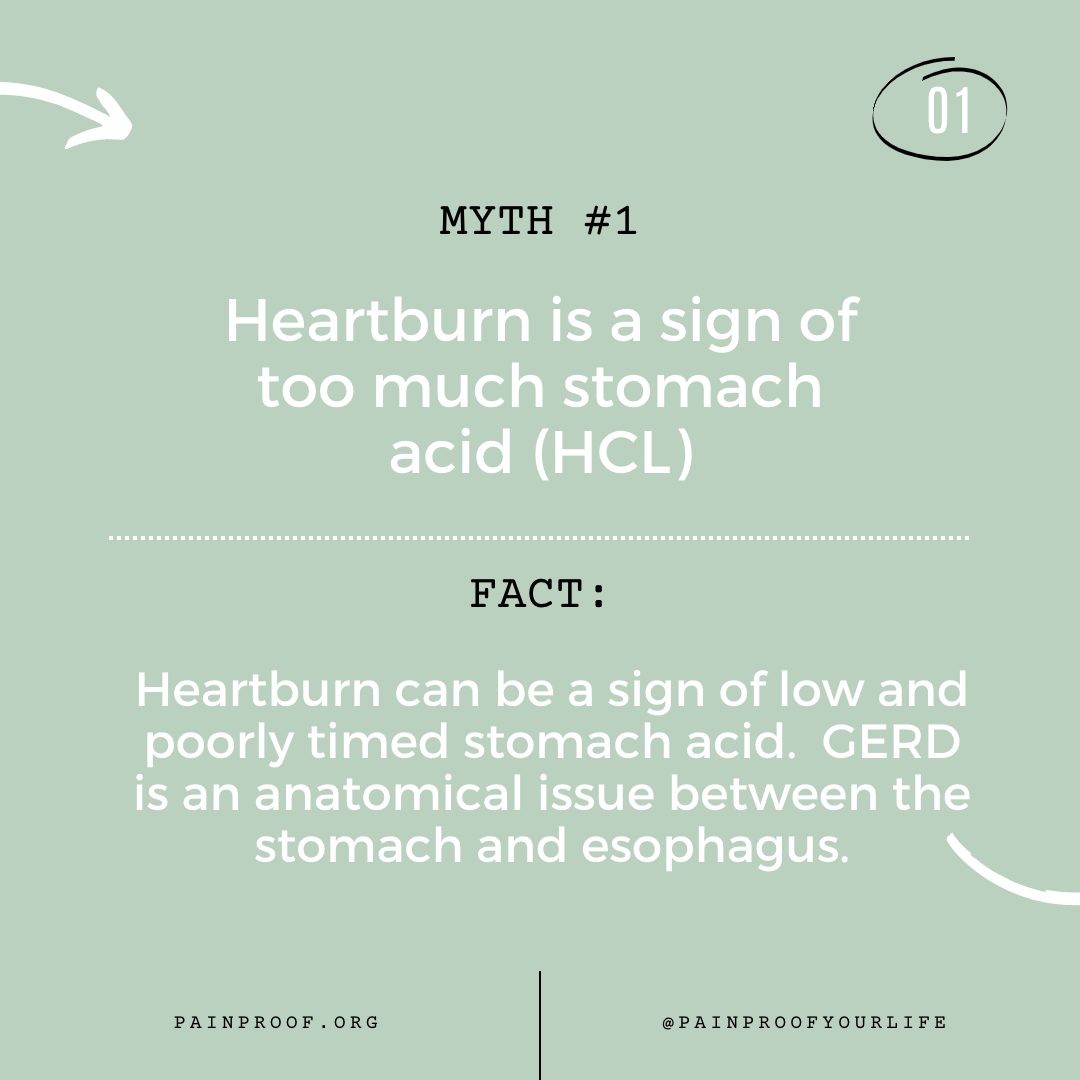
Myth #1: Heartburn is a sign of too much stomach acid
Fact: Heartburn can be a sign of low and/or poorly timed stomach acid.
Stomach acid should not exist in a constant state. Meaning, we want our stomach acid to rise and fall depending upon what is going on in our stomach. GERD is due to a poorly functioning sphincter (ring of muscle) that connects the stomach to the esophagus. We don’t want to prevent our body from making stomach acid; we want it to be at the right pH at the right time. When stomach acid is not at the right level, it can rebound inappropriately when food is added.
Ways to improve appropriate HCL levels:
-
Limit/remove alcohol
-
Address nutrient deficiencies (yes, this one can be a chicken/egg scenario)
-
Determine need for zinc, B vitamins, calcium (dietary), magnesium, potassium, & sodium
-
Remove intestinal mucous-irritating substances (alcohol and food sensitivies/allergies)
-
Eat enough animal protein
-
Reduce/Remove Acid blocking medications (see Myth #4)
-
Remove/Reduce use of NSAIDS (anti-inflammatories, including aspirin)
-
Reduce stress*
* Stress is something we all can tackle. When we are in a stress-full state, we are no longer in a ‘rest & digest’ state. Get this FREE download for specific strategies.
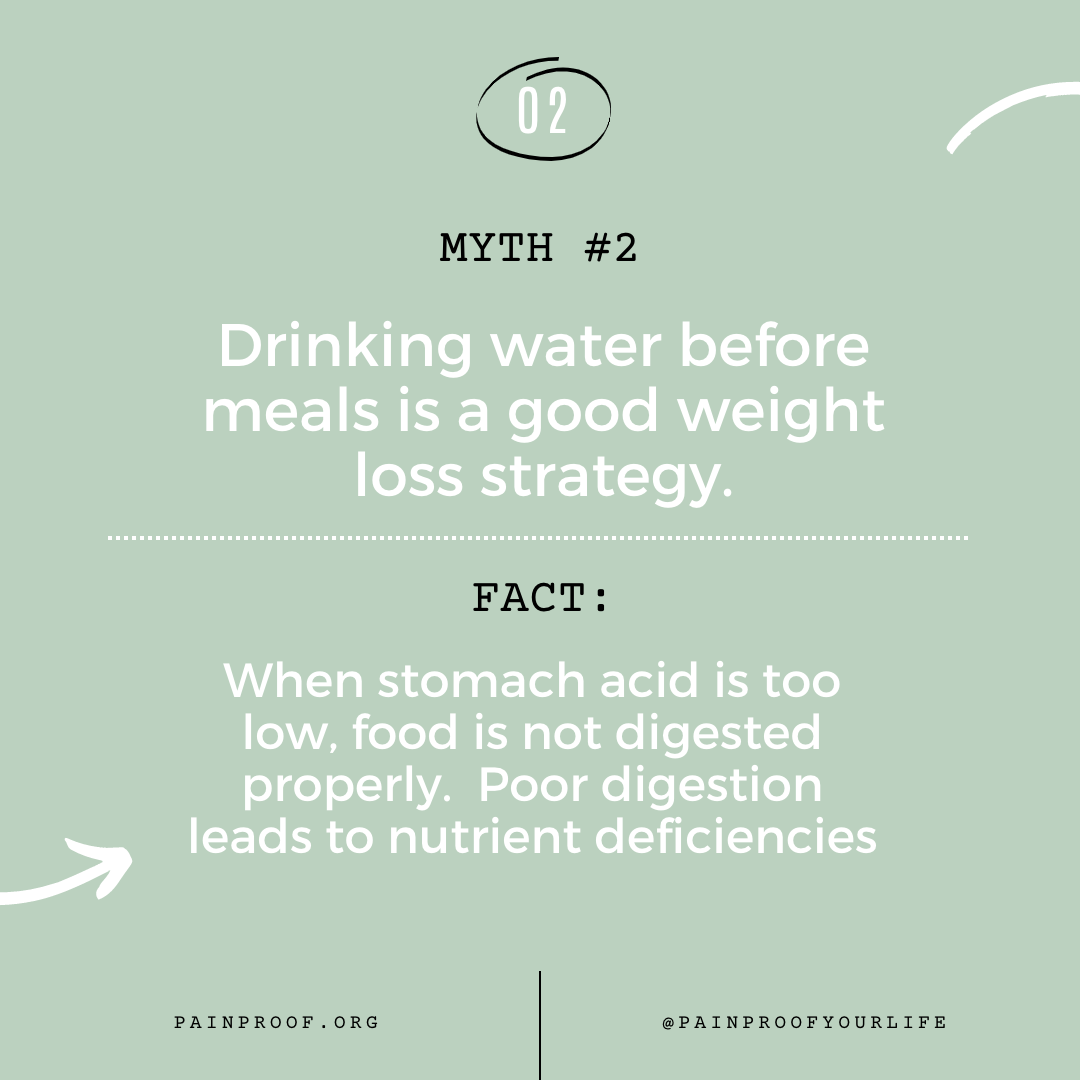
Myth #2: Drinking water before meals is a good weight loss strategy
Fact: When stomach acid too low, food is not digested properly. Poor digestion or incomplete digestion leads to nutrient deficiencies.
This is controversial topic for sure. Follow this logic and make your own decision.
The stomach has a lower pH level (more acidic) when empty than with food – but this is a relative concept. When food is introduced, the stomach becomes less acidic (higher pH) simply because there is something present to lower it. The pH veers towards neutral (pH =7), but doesn’t become basic (pH above 7).
Drinking too much water can lower the acidity of the stomach (higher pH) which means there isn’t enough acid to break down the food (or disinfect it).
When HCL is low, some nutrients will not be released or liberated from their bonds. Calcium, Iron and zinc need higher stomach acid to become available for absorption – especially if contain within fiber-containing foods. Here’s the kicker – we need Zinc as a building block to make stomach acid.
Myth #3: High stomach acid should be avoided
Stomach acid fluctuates. Timing is key!
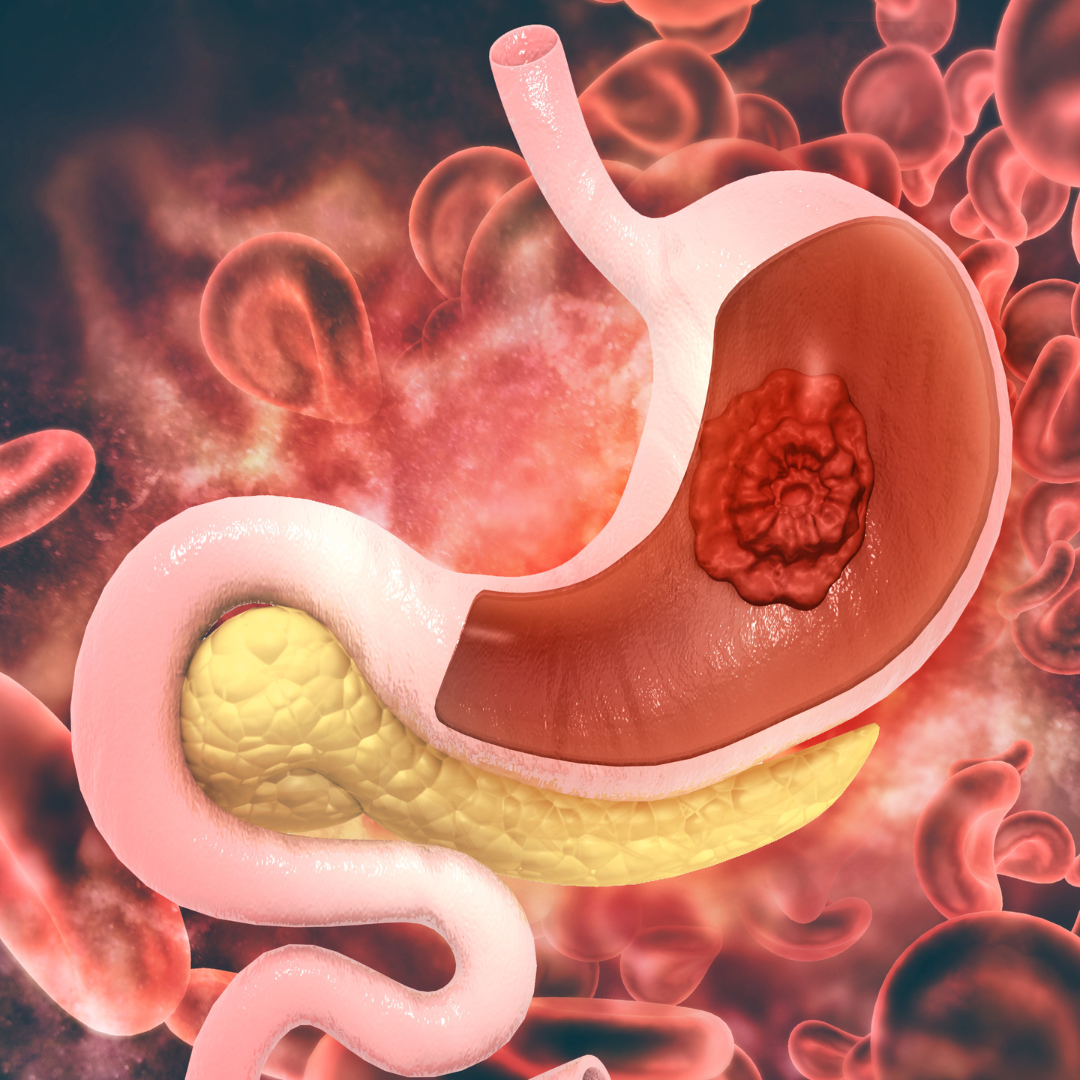
Our stomach acid is regulated primarily by the parasympathetic portion of our autonomic nervous system. Part of this process is regulating the increase or decrease of stomach acid (HCL). When we don’t have enough stomach acid, to start, we risk getting pathogens, viruses, and other invaders. We need HCL to activate pepsinogen into pepsin so the food we eat is disinfected. If those pesky invaders are not neutralized, they keep heading south with the food to cause problems.
In addition, without proper HCL levels protein digestion won’t even get started. So, if you’re someone who feels like meat ‘sits in your stomach’ or doesn’t settle well, low stomach acid might be a part of the problem.
Myth #4: It’s not harmful to take antacids daily
Antacids like TUMS, Prilosec, or Pepcid lower stomach acid and disrupt the intestinal flora. Addressing the root issue of indigestion is vital to fixing the problem. Masking symptoms often leads to bigger problems down the road. Proton pump inhibitors increase the risk of intestinal infections (like Clostridium difficile colitis) and leaky gut. When food is not fully digested in the early stages (i.e. your stomach) it can cause dysbiosis downstream and after the fact. Long term antacid use can also lead to osteoporosis, bone fractures, atrial fibrillation, dementia and pneumonia. (See a full list of potential side effects from Epocrates).
Common Adverse Reactions to Antacids (from Epocrates):
-
Headache
-
Abdominal Pain
-
Nausea
-
Diarrhea
-
Vomiting
-
Flatulence (gas)
-
Fever (in pediatric)
-
Upper Respiratory Infections
-
Vitamin B12 deficiency
-
Fundic gland polyps
So, let me ask you this:
Would you rather keep taking antacids or get to the root of the problem?
References:
Comments